The Clinical and Translational Science (CTS) Pilot Program invests in investigators with innovative ideas and established scientists expanding their domain expertise. We support pilot projects that will pilot innovative approaches for addressing important roadblocks in translational science with a focus on the Academic Learning Health System (aLHS). While addressing these translational roadblocks, these projects will also apply a fair lens and facilitate multidisciplinary, team-based, and patient-centric science that is broadly generalizable.
The CTS Pilot Program supports two RFAs each year: The Science of Translation RFA and the Translational Research RFA. Both RFAs aim to fund one-year pilot projects at $40,000 each.
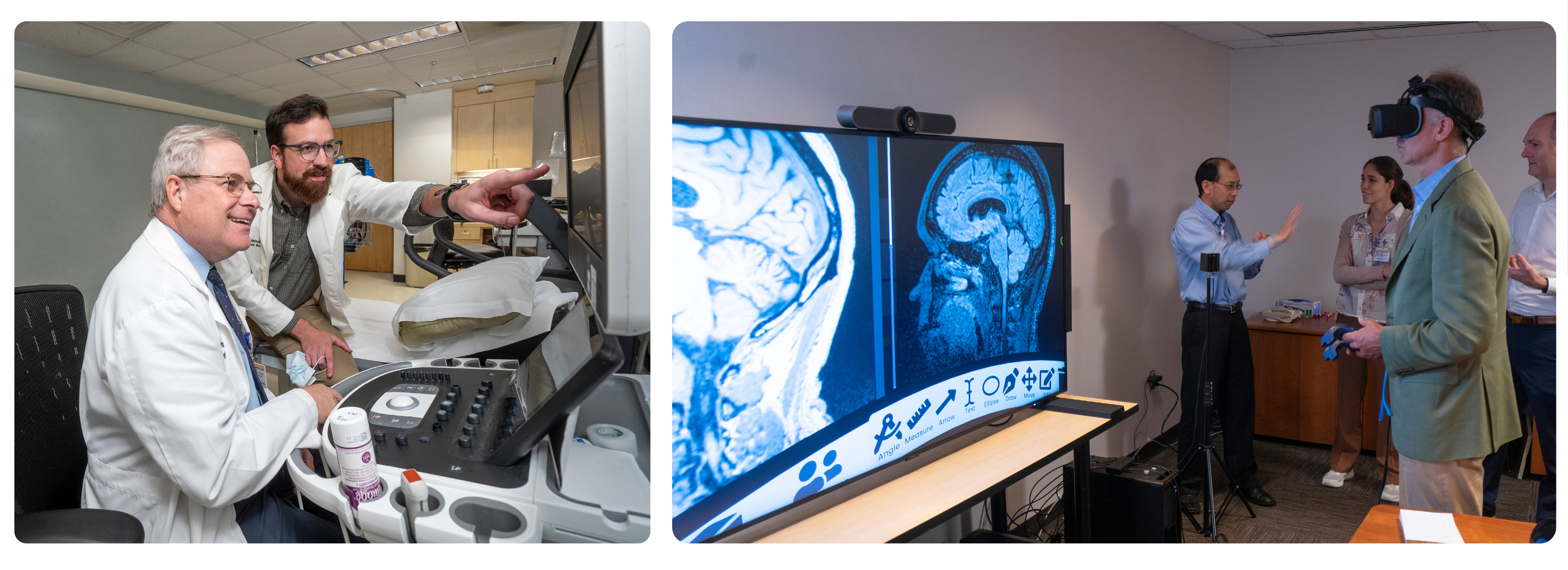
Pilot Award Examples Ignition Funds